Flexible laryngoscopy is viewing of the pharynx and larynx using a flexible laryngoscope (also called a nasopharyngolaryngoscope).
Flexible laryngoscopy is generally done to evaluate symptoms or disorders of the pharynx and larynx.
(See also Evaluation of the Patient With Nasal and Pharyngeal Symptoms and Overview of Laryngeal Disorders.)
Indications for Flexible Laryngoscopy
Laryngoscopy may be indicated for the evaluation of patients with the following:
Chronic cough
Chronic throat pain
Dysphagia
Dysphonia
Foreign body in the throat
Hoarseness or change in voice
Odynophagia
Sensation of a lump in the throat
Symptoms of aspiration (eg, coughing, choking, and wheezing progressing to fever; chest pain and shortness of breath if there is lung involvement)
Sometimes hemoptysis
In particular, patients at a high risk of head and neck cancer (eg, those who smoke heavily or those who regularly use alcohol) may benefit from laryngoscopy, especially if they have had hoarseness, sore throat, or ear pain for > 2 weeks. Patients who have had or require thyroid and parathyroid surgery should also undergo laryngoscopy to assess the function of the recurrent laryngeal nerve and to identify vocal cord paralysis.
Laryngoscopy can also be useful to evaluate the airway prior to orotracheal intubation.
Urgent laryngoscopy may be indicated in patients with stridor, epistaxis, and/or craniofacial trauma. Patients experiencing head and neck angioedema, especially those with lingual involvement, should be examined under direct laryngoscopy rather than mirror laryngoscopy (to assess involvement of tongue's base and the larynx and for airway management) (1).
Flexible laryngoscopy can be tried for patients who do not tolerate direct laryngoscopy.
Contraindications for Flexible Laryngoscopy
Absolute contraindications
Suspected epiglottitis
Relative contraindications
Stridor
Angioedema
Active epistaxis (as the endoscope is inserted through the nose) or an uncontrolled bleeding disorder
In patients with stridor or angioedema, stimulation of the laryngopharynx may cause worsening constriction and further compromise the airway (2). If laryngoscopy is essential (eg, to assess the airway), it should be performed in the controlled setting of an operating room and in the presence of a clinician skilled at difficult airway management (including surgical techniques) (1).
Complications of Flexible Laryngoscopy
Injury to the mucosa, which may cause bleeding
Laryngospasm and airway compromise
The procedure may cause gagging, coughing, and/or vomiting. Occasionally, the procedure may trigger a vasovagal reaction.
Equipment for Flexible Laryngoscopy
Gloves
Protective eyewear
Mask
Flexible laryngoscope (nasopharyngolaryngoscope) with light source
Nasal speculum
Water-soluble lubricants
Wall suction connected to a Frazier-tip catheter
Topical vasoconstrictor/anesthetic (eg, 4% cocaine, 0.05% oxymetazoline plus either 1% tetracaine or 4% lidocaine)Topical vasoconstrictor/anesthetic (eg, 4% cocaine, 0.05% oxymetazoline plus either 1% tetracaine or 4% lidocaine)
Cotton swabs or pledgets for nonspray topical decongestants and/or anesthetics
Additional Considerations for Flexible Laryngoscopy
Flexible laryngoscopy provides only a limited view of the subglottic larynx and proximal trachea. To assess these regions, use another procedure, such as bronchoscopy.
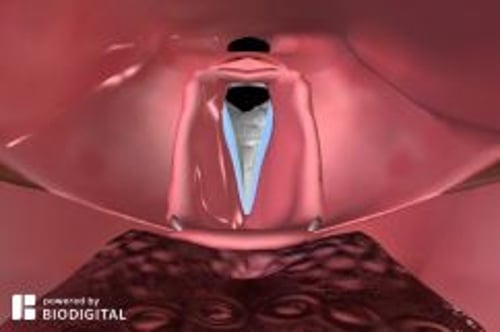
Relevant Anatomy for Flexible Laryngoscopy
The pharynx includes the nasopharynx, oropharynx, and hypopharynx.
The larynx connects the pharynx to the trachea and is suspended from the hyoid bone. It includes 3 single and 3 paired cartilage structures: single (epiglottis, thyroid, and cricoid) and paired (arytenoid, cuneiform, and corniculate). The larynx extends from the tip of the epiglottis down to the inferior aspect of the cricoid cartilage and includes the vocal folds.
Positioning for Flexible Laryngoscopy
The patient should sit upright with the head against a headrest, and leaning forward slightly.
Legs should not be crossed.
Step-by-Step Description of Flexible Laryngoscopy
Preparation
Check that the laryngoscope and its light source and suction, are working properly.
Adjust eyepiece focus (use letters such as on medication or equipment packaging).
Check both nares and use the one that appears more widely patent.
Hold the nares open with a nasal speculum. Insert the speculum with the handle parallel to the floor and open the speculum vertically; stabilize your hand by placing one or two fingers against the patient's nose.
Apply the topical vasoconstrictor/anesthetic; then remove the speculum.
Procedure
Do the following approximately 5 to 15 minutes after the application of the vasoconstrictor/anesthetic:
Lubricate the laryngoscope tip with water-soluble lubricant.
Insert the laryngoscope tip into the nose and advance it slowly adjacent to the inferior turbinate (either above or below) and parallel to the floor of the nose.
Advance it into the nasopharynx, inspecting the eustachian tube opening in the lateral nasopharynx and the adenoid tissue on the posterior wall.
Tell the patient to breathe through the nose (which makes the soft palate drop).
Use the thumb control on the laryngoscope to flex the tip down to go past the palate, and then straighten to avoid curling forward into the uvula.
Inspect the base of the tongue, valleculae, epiglottis, piriform sinuses, arytenoids, false and true vocal cords, and the larynx below the vocal cords.
Do not pass the laryngoscope through the vocal cords because contact can cause laryngospasm.
Fully inspect the vocal cords.
Instruct the patient to say "eeee," which will contract the vocal cords and allow more thorough inspection; doing so will also permit assessment of vocal cord function.
Avoid touching the mucosa or epiglottis because this may provoke a gag reflex.
Gently withdraw the laryngoscope.
Aftercare for Flexible Laryngoscopy
Instruct the patient to avoid eating and drinking for at least 20 minutes after the procedure to prevent aspiration due to residual laryngopharyngeal anesthesia.
Warnings and Common Errors for Flexible Laryngoscopy
Inserting the laryngoscope too forcefully, causing bleeding and/or discomfort
Losing situational awareness of the direction of the scope tip
Using too little anesthesia or vasoconstrictor
Tips and Tricks for Flexible Laryngoscopy
Give the patient a tissue prior to the procedure because involuntary tear production may occur.
Remind the patient to breathe normally during the procedure because some patients reflexively hold their breath.
Before inserting the laryngoscope, refamiliarize yourself with the tip controls.
Ask the patient not to swallow during the procedure unless directed to help clear the laryngoscope.
References
1. Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136(1):31-81. doi:10.1097/ALN.0000000000004002
2. Moellman JJ, Bernstein JA, Lindsell C, et al. A consensus parameter for the evaluation and management of angioedema in the emergency department. Acad Emerg Med. 2014;21(4):469-484. doi:10.1111/acem.12341