Scapular manipulation repositions the glenoid fossa rather than the humeral head. It requires less force than many other methods and can sometimes be performed without analgesia.
(See also Overview of Shoulder Dislocation Reduction Techniques, Overview of Dislocations, and Shoulder Dislocations.)
Scapular manipulation is a preferred technique because it is gentle, easy to perform, and free of complications.
Indications for Scapular Manipulation
Anterior dislocation of the shoulder
Reduction should be attempted soon (eg, within 30 minutes) after the diagnosis is made.
Reduction should be attempted immediately if an associated neurovascular deficit or skin tenting (due to a displaced bone fracture, or, less commonly, a fracture-dislocation, with potential for skin penetration or breakdown) is present. If an orthopedic surgeon is unavailable, closed reduction can be attempted, ideally using minimal force; if reduction is unsuccessful, it may need to be performed in the operating room under general anesthesia.
Open dislocations require surgery, but closed reduction techniques and immobilization should be performed as interim treatment if the orthopedic surgeon is unavailable and a neurovascular deficit is present.
Contraindications to Scapular Manipulation
Contraindications to simple closed reduction:
Greater tuberosity fracture with > 1 cm displacement
Significant Hill-Sachs deformity (≥ 20% humeral head deformity due to impaction against glenoid rim)
Surgical neck fracture (below the greater and lesser tuberosities)
Bankart fracture (anteroinferior glenoid rim) involving a bone fragment of over 20% and with glenohumeral instability
Proximal humeral fracture of 2 or more parts
These significant associated fractures require orthopedic evaluation and management, because of the risk of the procedure itself increasing displacement and injury severity.
Other reasons to consult with an orthopedic surgeon prior to reduction include:
The joint is exposed (ie, an open fracture or dislocation where bone or fracture segments penetrate the skin).
The patient is a child, in whom a physeal (growth plate) fracture is often present; however, if a neurovascular deficit is present, reduction should be performed immediately if the orthopedic surgeon is unavailable.
The dislocation is older than 7 to 10 days, due to an increased risk of damaging the axillary artery during the reduction, especially in older patients.
Complications of Scapular Manipulation
Complications are uncommon with the scapular manipulation technique.
Equipment for Scapular Manipulation
Intra-articular anesthetic*: 20 mL of 1% lidocaine, 20-mL syringe, 5 cm (2-inch) 20-gauge needle, antiseptic solution (eg, chlorhexidine, povidone iodine), gauze padsIntra-articular anesthetic*: 20 mL of 1% lidocaine, 20-mL syringe, 5 cm (2-inch) 20-gauge needle, antiseptic solution (eg, chlorhexidine, povidone iodine), gauze pads
Shoulder immobilizer or sling and swathe
* Patients are offered analgesia; however, if the patient wishes, one reduction attempt without analgesia may be performed.
Additional Considerations for Scapular Manipulation
Reduction attempts are more likely to succeed if patients are calm and can relax their muscles. Analgesia and sedation help patients relax, as may external distractions such as pleasant conversation.
Procedural sedation and analgesia (PSA) is often needed if substantial pain, anxiety, and muscle spasm impede the procedure.
Regional anesthesia can be used (eg, ultrasound-guided interscalene nerve block) but has the disadvantage of limiting post-reduction neurologic examination.
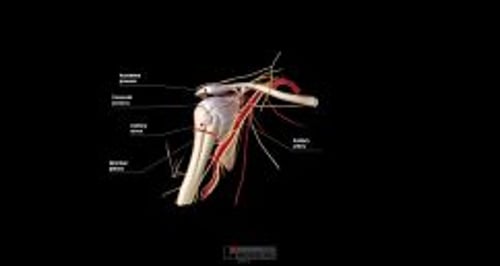
Relevant Anatomy for Scapular Manipulation
In most anterior dislocations, the humeral head is trapped outside and against the anterior lip of the glenoid fossa. Reduction techniques must distract the humeral head away from the lip and then return the humeral head into the fossa.
Deficits of the axillary nerve are the most frequent nerve deficits with anterior shoulder dislocations. They often resolve within several months, sometimes soon after the shoulder reduction.
Axillary artery injury is rare with anterior shoulder dislocations and suggests possible concurrent brachial plexus injury (because the brachial plexus surrounds the artery) (1).
Positioning for Scapular Manipulation
Position the patient sitting upright (easiest) or lying prone. If sitting upright, raise the head of the stretcher 90° and seat the patient sideways on the stretcher with the unaffected side leaning against the upright portion of the stretcher.
Step-by-Step Description of Scapular Manipulation
Neurovascular examination
Perform a preprocedure neurovascular examination of the affected arm, and repeat the examination after each reduction attempt. Generally, testing motor function is more reliable than testing sensation, partly because cutaneous nerve territories may overlap. Assess the following:
Distal pulses, capillary refill, cool extremity (axillary artery)
Light touch sensation of the lateral aspect of the upper arm (axillary nerve), thenar and hypothenar eminences (median and ulnar nerves), and dorsum of the 1st web space (radial nerve)
Shoulder abduction against resistance, while feeling the deltoid muscle for contraction (axillary nerve): However, if this test worsens the patient's pain, omit it until after the shoulder has been reduced.
Thumb-index finger apposition ("OK" gesture) and finger flexion against resistance (median nerve)
Finger abduction against resistance (ulnar nerve)
Wrist and finger extension against resistance (radial nerve)
Intra-articular analgesia
If a cooperative patient chooses to try reduction without analgesia, only one such attempt should be made. To administer intra-articular analgesia:
The needle insertion site is approximately 2 cm inferior to the lateral edge of the acromion process (into the depression created by the absence of the humeral head).
Swab the area with antiseptic solution, and allow the antiseptic solution to dry for at least 1 minute.
Optional: Place a skin wheal of local anesthetic (≤ 1 mL) at the site.
Insert the intra-articular needle perpendicular to the skin, apply back pressure on the syringe plunger, and advance the needle medially and slightly inferiorly approximately 2 cm.
If any blood is aspirated from the joint, hold the needle hub motionless, switch to an empty syringe, aspirate all of the blood, and re-attach the anesthetic syringe.
Inject 10 to 20 mL of anesthetic solution (eg, 1% lidocaine).Inject 10 to 20 mL of anesthetic solution (eg, 1% lidocaine).
Wait for analgesia to occur (up to 15 to 20 minutes) before proceeding.
Reduce the shoulder—Scapular manipulation
If the patient is seated upright, have an assistant face the patient, use one hand to apply gentle traction to the affected arm while holding it in 90° of flexion, and use the assistant's other arm (outstretched and with hand placed on the clavicle of the affected side) to provide a counterforce.
If the patient is prone, the affected arm hangs over the side of the stretcher. Gentle downward traction can be applied manually by an assistant or by attaching weights.
Regardless of patient position, slight external rotation of the affected arm may facilitate reduction.
Manipulate the scapula: Regardless of patient position, use the digits of one hand to stabilize the superior aspect of the scapula along the medial border while using both thumbs to gently and gradually apply a medial and dorsal force to the inferior tip of the scapula. Attempt to slightly displace the tip dorsally while pushing it toward the spine. Reduction usually occurs within several minutes and may be subtle or even go unnoticed.
Optional: "Best-of-both" technique
The "best-of-both" (BOB) technique combines the scapular manipulation and the external rotation techniques (2).
Raise the head of the stretcher 90° and seat the patient sideways on the stretcher with the unaffected side leaning against the head of the stretcher.
Hold the affected upper arm adducted against the patient's side.
Gently hold the patient's wrist, keeping the elbow flexed 90° and the forearm neutral (ie, thumb pointing cephalad).
Apply gentle axial traction caudally and externally rotate the shoulder.
Have an assistant manipulate the scapula as described above by stabilizing the superior aspect of the scapula along the medial border and gradually apply a medial and dorsal force to the inferior tip of the scapula.
Aftercare for Scapular Manipulation
Successful reduction is preliminarily confirmed by restoration of a normal round shoulder contour, by decreased pain, and by the patient's renewed ability to reach across the chest and place the palm of the hand upon the opposite shoulder.
Immobilize the shoulder with a sling and swathe or with a shoulder immobilizer.
Because the joint can spontaneously dislocate after successful reduction, do not delay immobilizing the joint.
Perform a post-procedure neurovascular examination. A neurovascular deficit warrants immediate orthopedic evaluation.
Perform post-procedure radiographs to confirm proper reduction and identify any coexisting fractures.
Arrange orthopedic follow-up.
Warnings and Common Errors for Scapular Manipulation
Apparent shoulder dislocation in a child is often a fracture involving the growth plate, which tends to fracture before the joint is disrupted.
Tips and Tricks for Scapular Manipulation
The lateral border of the scapula is located more laterally than one might expect.
The scapular manipulation technique may be more difficult in larger patients having obscure anatomic landmarks.
Operators not familiar with this technique may prefer the prone patient position because of the ease of identifying the scapular landmarks.
In patients who return with increased pain within 48 hours after a reduction, hemarthrosis is likely (unless the shoulder has again dislocated). Aspirate the blood from the joint space (see How To Do Arthrocentesis of the Shoulder).
References
1. Perlmutter GS, Apruzzese W. Axillary nerve injuries in contact sports: recommendations for treatment and rehabilitation. Sports Med. 1998;26(5):351-361. doi:10.2165/00007256-199826050-00005
2. Sagarin, MJ: Best of both (BOB) maneuver for rapid reduction of anterior shoulder dislocation. J Emerg Med 29(3):313-316, 2005.